Resources
We are an organization dedicated to supporting individuals with OCD, as well as their families, healthcare providers, and committed young individuals. The OCDNetworkSG has been offering a range of services including support programs, collaborative events, and fostering a close-knit community for those affected by this condition.


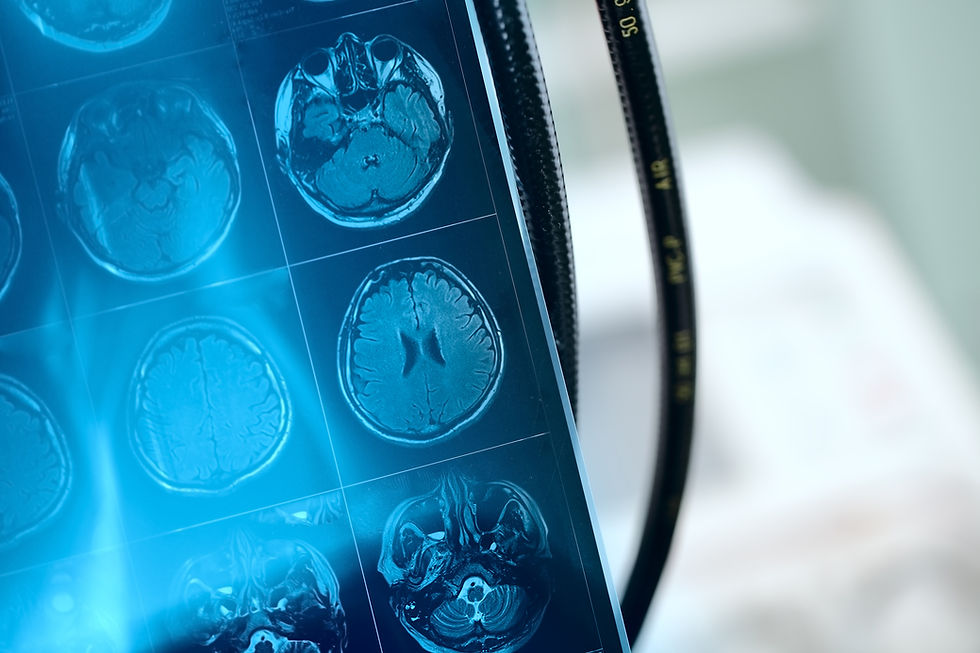
Brain Circuitry
Neuroimaging investigations conducted on patients diagnosed with OCD have revealed elevated neural activity and heightened blood circulation within distinct regions of the brain.
Brain Chemistry
Serotonin, a neurotransmitter present in brain cells, plays a crucial role in transmitting information between neurons. Research indicates an inequity of serotonin levels within the brains of individuals living with OCD.
Causes of OCD
There are a number of factors that can contribute to the development of OCD

Genetics
Research conducted on family dynamics has provided evidence indicating a higher susceptibility to developing OCD among immediate relatives of individuals affected by the disorder, as opposed to the general population. Furthermore, studies have revealed that there exists an 80% concordance rate for monozygotic twin pairs and a 50% concordance rate for dizygotic twin pairs.

Stress/ Life Events
Significant life occurrences, such as the loss of a loved one or experiencing high levels of stress, can activate symptoms of OCD in individuals who are predisposed to develop this condition. Furthermore, positive events like childbirth may also serve as potential catalysts for the manifestation of this underlying disorder.
Infection
Research conducted on family dynamics has provided evidence indicating a higher susceptibility to developing OCD among immediate relatives of individuals affected by the disorder, as opposed to the general population. Furthermore, studies have revealed that there exists an 80% concordance rate for monozygotic twin pairs and a 50% concordance rate for dizygotic twin pairs.

What is OCD?
Obsessive compulsive disorder (OCD), a manageable neurological psychiatric condition, manifests through repetitive behaviors (compulsions/rituals) and unwanted intrusive thoughts (obsessions). These compulsions are undertaken in an individual's endeavor to alleviate obsessions and minimize distress. The time-consuming nature of OCD obsessions and compulsions, coupled with the substantial emotional turmoil they induce, can impede daily activities and interpersonal connections.
How Common is OCD?
The estimated global prevalence rates of Obsessive-Compulsive Disorder (OCD) stand at 1.5% for women and 1% for men over their lifetime. In Singapore, the results from the 2016 Singapore Mental Health Study indicate that the prevalence rates of OCD are slightly higher, with figures of 3.6% and 2.9% for lifetime and 12-month occurrences respectively. This means that approximately one in every twenty-eight individuals in Singapore will experience OCD at some point during their lives. Remarkably, OCD ranks among the top three most commonly occurring mental health conditions in Singapore, trailing only Alcohol Abuse and Major Depressive Disorder (MDD).
While OCD can manifest itself at any age, it typically commences either during childhood between eight and twelve years old or later on during adolescence or early adulthood. Once established, this condition often persists throughout a person's entire life span.

Types of OCD

Counting & Checking
Counting and checking are performed in an effort to address obsessive and fearful thoughts or to prevent something bad from happening. Counting can be associated both with the need to avoid danger and the obsession for symmetry and exactness. Checking rituals often involve an impulse to check items such as door locks, light switches, taps, and stoves.

Fear Of Harm
Harming Intrusive Thoughts consist of unwanted thoughts or images that one might harm themselves or someone else on impulse. Individuals within this OCD subtype have no intent to hurt themselves or others and the intrusive thought or image often causes a significant amount of anxiety and disturbance for these individuals.
Treatments for OCD
Where to Seek Treatment
Many other restructured hospitals and clinics within the community also offer treatment for OCD.
What Families Should Know
Your loved one’s OCD isn’t anyone’s fault. OCD is a neurological problem. The obsessions are involuntary and the person experiencing them cannot simply control or get rid of them by an effort of will. Family members, caregivers and friends often feel helpless, not knowing how to reach out or what to do to help their loved one. They often respond to OCD with antagonistic or accommodating behaviours, both of which may cause OCD symptoms to flare up. People with OCD often feel even more distress when they are subjected to criticism or blame.
Here’s what you can do to help your loved one living with OCD:
The more you know about OCD, the better equipped you will be to avoid pitfalls, cope with challenges and, most importantly, help your loved one.
Erosion of a person’s motivation through OCD can be a barrier to their seeking treatment. To manage OCD in a supportive way, share with your loved one what you know about the disorder, and provide information about both the medications and Exposure and Response Prevention Therapy (ERP). Help your loved one to access these treatments.
Parents often feel they are responsible for their child’s OCD, when it is something over which they truly have no control. Once you accept that OCD is nobody’s fault, you will be able to take action that is honest and helpful, and not clouded by ideas of what you could or should have done.
Remember that everyone progresses at their own pace, and your loved one is not weaker or stronger than another OCD patient based on the speed of his or her recovery. Some may have more setbacks than others, even in treatment. When you stop making comparisons, you can truly be happy for your loved one when they accomplish their goals. It is important to be patient, encouraging and supportive.
Avoid criticizing or mocking your loved one’s symptoms. Do not suddenly spring a situation on them in which they are bound to feel anxious. Learn how you can be supportive without accommodating your loved one’s compulsions.
Work closely with the psychiatrist, psychologist and other mental health professionals to help your loved one fight OCD.
However successful or unsuccessful the efforts made have been, praise your loved one for standing up to his or her OCD. Acknowledging their efforts and recognizing improvements (even when the wins seem small), will encourage your loved one to keep trying.
Keep communication simple, and avoid complicated explanations.
OCD treatment is hard work, often exhausting for your loved ones. Remind them of their motivation and their recovery goals, as this may encourage them to continue the treatment progress so that they can get their life back.
Be sure to follow the medication instructions that have been prescribed. Do not try to reduce or increase the dosage of the medication without consulting the doctor. All medications have side effects that range in severity. If you have any concerns, you could periodically (if your loved one agrees to this) attend the doctor’s appointment with him/her, so that you can ask questions, learn about side effects and report any behavioural changes that you have noticed.
Do not change your family routine to accommodate your loved one’s OCD behaviours. Discuss your expectations ahead of time and do not engage in boundary discussions during stressful events. Remember that it is in the individual’s best interests to tolerate exposure to their fears and be reminded of others’ needs. As they begin to return to normal functioning, their wish to do more will increase.
Share and listen to other caregivers how they handle their loved ones’ OCD behaviours. Get feedback about how you can better manage your family member’s OCD demands and/or support them in their recovery journey.
Myths about OCD
Hoarding is part of OCD
At one time, hoarding was considered part of OCD. In recent years, however, it has been recognised that in many cases hoarding is entirely separate from OCD; and in the DSM-5, hoarding disorder has been categorised as a condition in its own right, usually referred to as “Compulsive Hoarding Disorder”. One feature characterising hoarding disorder as different from OCD is that frequently those living with it respond in ways very different from people with OCD. For example, most people with OCD realise something is wrong and usually want to get better. Hoarders often refuse to accept they have a problem and either do not want to get better or will not admit to experiencing any difficulty.
OCD is an addiction
Sex, gambling, drugs, alcohol, shopping may be compelling obsessions/compulsions – but these are NOT OCD. They start out as pleasurable interests adopted without any anxiety or fear of consequences, and would therefore never be part of clinical OCD.
You should feel better after therapy
Making room for unwanted thoughts and feelings and facing your fears are critical aspects of ERP treatment. Instead of making you feel good, the goal is to help you feel more empowered to manage OCD for the long haul, and thereby lessen its impact on your life.
Accepting your thoughts means that you have to agree with them or like having them
The goal of the therapy is to learn to adopt an attitude in which “forbidden” or “taboo” thoughts are deemed unimportant and the content of OCD-related thoughts is recognised as irrelevant. In fact, it is the struggle to get away from the thoughts or make them go away that brings them back more frequently and with added intensity. Remember, nearly everyone experiences intrusive thoughts, whether or not they have OCD – it is how we respond to them that matters!
The goal of an ERP treatment is to eliminate intrusive thoughts and anxiety, or to cure OCD
OCD cannot be cured but it can be successfully managed! By equipping yourself with the tools and expertise to better manage unwanted internal experiences, and by consistently making choices that reflect your values not your OCD fears, you can feel more empowered to handle whatever variation of OCD may arise for you in the future.
If you face situation you fear, this will worsen your condition and increase your anxiety
ERP helps to build up your tolerance of uncertainty and the accompanying discomfort. By doing the exposure exercises repeatedly, the brain grows to realise that even though these situations or “triggers” feel dangerous, they no longer need to be treated as such. The brain also learns that anxiety is not long-lasting and will dissipate even if rituals are not performed. We face uncertainty and take risks every day. The reality is that nothing in life is certain and we can never ensure that there will be zero threats, even outside the framework of the OCD theme.
Medication can cure OCD instantly
It is important to recognise that medications for OCD take time to work and require consistency in approach. Irrespective of the medication path you choose, in order to optimise your treatment you will need to take your medication daily and at a therapeutic dose recommended by your doctor. Research tells us that it can take up to three months in some cases to even start experiencing a reduction in OCD symptoms. Your doctor may consider decreasing the dosage or discontinuing your medication if your OCD symptoms have improved significantly and you have acquired sufficient ERP skills to help you overcome your OCD competently on your own.
People with OCD have no hopes & cannot live normal lives
People with OCD can live happy and fulfilled lives with proper treatment. A CBT-based intervention known as Exposure and response prevention (ERP) is regarded as the gold standard treatment, as scientists consider it to be highly effective in treating OCD. People with OCD can also benefit from medications, family therapy and the love and support of their loved ones.
OCD has its origin in your childhood
Many people mistakenly believe that people who exhibit signs of OCD grew up in dysfunctional homes and have poor self-esteem as a result. Studies have shown that what happened in one’s childhood has very little to do with having OCD when you grow up. It is noted however that OCD does run in families and scientists suggest that genetic factors, as well as personal experiences, may play at least some part in its development.
All neat and clean freaks have OCD.
One common sign of OCD is an obsession with cleanliness – such as constantly washing your hands or excessively cleaning household items. But a preoccupation with cleanliness could also be a personality trait. If it is a personality trait, you have control – you can choose whether or not to do it. If you have OCD, you are doing it out of unrelenting, debilitating anxiety or distress.
People with OCD believe their obsessive thoughts.
Most people with OCD are aware that their obsessions and compulsions are irrational. Indeed, this is part of the torment of OCD: their insight does little to make compulsive behaviours easier to resist. Often, sufferers feel they have no choice and feel compelled to perform these compulsive rituals to negate their anxiety or prevent something bad from happening.
Stress causes OCD
It is totally wrong to imagine that people with OCD can just relax and “turn off” their obsessive thoughts. It is not that simple. Even simple habits are difficult to change. OCD incites uncontrollable fears and distress. While stressful situations can cause people’s OCD symptoms to flare up, stress alone does not cause this to happen.
The obsessions in OCD leads to aggressive, violent & inappropriate behaviour
Some obsessions can have disturbing, violent, sexual or taboo-related contents. Like all other obsessions, these are involuntarily experienced and completely unwanted and uninvited. People with OCD typically do NOT seek to act out violent, aggressive or sexual obsessions; they are, rather, highly disturbed by them and experience them as contrary to their sense of self (this is called “ego-dystonic”). Compulsions performed to combat such obsessions do NOT involve acting out obsessions. On the contrary, the compulsions are based on efforts to neutralise or undo the obsessions, or on checking to ensure that nobody has been hurt.








